Exercise Electrocardiogram
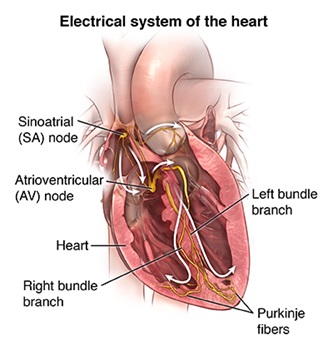
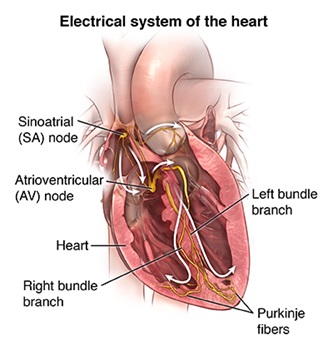
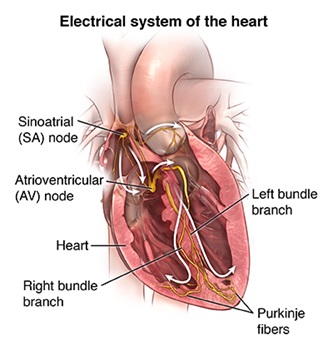
An electrocardiogram (ECG) is a simple and fast test to evaluate the heart. For this test, small, plastic patches that stick to the skin (electrodes) are placed at certain spots on the chest, arms, and legs. The electrodes are connected to an ECG machine by wires. Then, the electrical activity of the heart is measured, interpreted, and printed out. No electricity is sent into the body.
Natural electrical impulses coordinate contractions of the different parts of the heart to keep blood flowing the way it should. An ECG records these impulses to show how fast the heart is beating, the rhythm of the heart beats (steady or irregular), and the strength and timing of the electrical impulses as they move through the different parts of the heart. Changes in an ECG can be a sign of many heart-related conditions.
An exercise ECG, sometimes known as a stress test or exercise test, is done to assess the heart's response to stress or exercise. In this test, the ECG is recorded while you are exercising on a treadmill or stationary bike. An ECG tracing will be taken at certain points during the test to compare the effects of increasing stress on the heart. Periodically, the incline and treadmill speed will be increased to make exercise more difficult during the test. If you are riding a bike, you will pedal faster against increased resistance. In either case, you will exercise until reaching a target heart rate (determined by the healthcare provider based on age and physical status) or until you are unable to continue due to tiredness, shortness of breath, chest pain, or other symptoms.
Why might I need an exercise electrocardiogram?
Some reasons for your healthcare provider to request an exercise electrocardiogram (ECG) include:
- To assess stress or exercise tolerance if your doctor thinks you have coronary artery disease (blocked arteries in the heart)
- To determine limits for safe exercise before starting a cardiac rehab program or when recovering from a cardiac event, such as a heart attack (myocardial infarction, or MI) or heart surgery
- To assess heart rhythm and electrical activity during exercise
- To evaluate heart rate and blood pressure during exercise
There may be other reasons for your healthcare provider to recommend an exercise ECG.
What are the risks of an exercise electrocardiogram?
Because of stress on the heart during the test, there is a small chance for:
- Chest pain
- Heart attack
- High blood pressure
- Irregular heartbeats
- Dizziness
- Nausea
- Tiredness
- Passing out
- Cardiac arrest
- Serious heart rhythm problems.
It may be uncomfortable when the sticky electrodes are taken off. If the electrode patches are left on too long they may cause skin irritation.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
Certain factors or conditions may interfere with or affect the results of an exercise ECG including:
- Eating a heavy meal before the test
- Caffeine intake before the test
- Smoking or using other tobacco products before the test
- High blood pressure
- Electrolyte imbalances, such as too much or too little potassium, magnesium, or calcium in the blood
- Certain medicines, such as beta-blockers, that may make it difficult to increase the heart rate to the target level
- Heart valve disease
- Enlarged heart
- Arrhythmias
How do I get ready for an exercise electrocardiogram?
Tell your healthcare provider if you have:
- Aneurysm
- Uncontrolled chest pain (unstable angina)
- Severe heart valve disease (malfunction of one or more of the heart valves)
- Severe heart failure
- Recent heart attack (myocardial infarction or MI)
- Severe high blood pressure
- Uncontrolled irregular heartbeats
- Inflammation or infection of the sac that surrounds the heart (pericarditis)
- Low red blood cell count (severe anemia)
- A pacemaker
- Orthopedic issues that keep you from doing certain exercises
Here are other steps to get ready
- Your healthcare provider or the technician will explain the test to you and let you ask questions.
- You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if anything is not clear.
- You will be asked to fast (not eat or drink) for a few hours before the test.
- Don't smoke or use any other form of tobacco for 2 hours before the test.
- Tell your healthcare provider if you are pregnant or think you could be.
- Tell your healthcare provider of all medicines (prescription and over-the-counter), vitamins, herbs, and supplements that you are taking.
- You may be asked to hold certain medicines before the test, such as beta-blockers. Your healthcare provider will provide specific instruction.
- Wear comfortable walking shoes and loose-fitting pants or shorts.
- If you use an inhaler for asthma or other breathing problems, bring it to the test.
- Based on your medical condition, your healthcare provider may request other specific preparation.
What happens during an exercise electrocardiogram?
An exercise electrocardiogram (ECG) may be done on an outpatient basis or as part of your hospital stay. Tests may vary depending on your condition and your healthcare providers practice.
Generally, an exercise ECG follows this process:
- You will be asked to remove any jewelry or other objects that may interfere with the test.
- You will be asked to open your shirt in the front or remove your shirt. The technician will ensure your privacy by covering you with a sheet or gown and exposing only the necessary skin.
- If your chest is very hairy, the technician may shave or clip small patches of hair, as needed, so that the electrodes will stick closely to your skin.
- Electrodes will be attached to your chest and belly (abdomen).
- The wires will be attached to the electrodes.
- Once the wires are attached, the technician may enter identifying information about you into the machine's computer.
- A blood pressure cuff will be put on your arm while you are sitting down. An initial, or baseline, ECG and blood pressure readings will be taken while you are sitting down and standing up.
- You will be instructed on how to walk on the treadmill or use the bike.
- Let your healthcare provider know if you start to have any chest pain, dizziness, lightheadedness, extreme shortness of breath, nausea, headache, leg pains, or any other symptoms during exercise.
- You will start to exercise at a minimal level. The intensity of the exercise will be slowly increased.
- ECG and blood pressure readings will be taken periodically to measure how well your heart and body are responding to the exercise.
- The length of time you will exercise is based on a target heart rate (determined by the healthcare provider based on your age and physical condition) and your own exercise tolerance. Exercise duration is an important part of the stress test result. The test may be stopped if you develop severe symptoms, such as chest pain, dizziness, nausea, severe shortness of breath, severe tiredness, or elevated blood pressure.
- Once you have completed the exercise part of the test, the rate of exercise will be slowed for a "cool down" to help avoid any nausea or cramping from suddenly stopping.
- You will sit in a chair and your ECG and blood pressure will be monitored until they return to normal or near-normal. This may take 10 to 20 minutes.
- Once your ECG and blood pressure readings are acceptable, the ECG electrodes and blood pressure cuff will be removed. You may then get dressed.
What happens after an exercise electrocardiogram?
You should be able to go back to your normal diet and activities, unless your healthcare provider tells you differently.
Generally, there is no special care needed after an exercise ECG.
You may feel tired for several hours or longer after the test, particularly if you don't normally exercise. Otherwise, you should feel normal within a few hours after the exercise ECG. If you feel tired for more than a day, contact your healthcare provider.
Tell your healthcare provider if you develop any signs or symptoms (such as chest pain, shortness of breath, dizziness, or fainting).
Your healthcare provider may give you other instructions after the test, depending on your particular situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how you will get the results
- Who to call after the test or procedure if you have questions or problems
- How much you will have to pay for the test or procedure
Find a Doctor
- Coronary Angiography
- Cardiac Disease
- Cardiovascular Disease
- carotid artery stenting
- Laser Atherectomy
- Laser Ablation
- Dyslipidemia and Hypertension
- Dyslipidemia
- Treatment of Bypass Graft Disease with Distal Protection Devices
- Intravascular Brachytherapy
- Intravascular Ultrasound (IVUS)
- Ischemic Heart Disease
- Chronic Total Occlusions
- Chronic Total Coronary Occlusion
- Coronary Heart Disease
- Coronary Artery Disease
- Coronary Artery Bypass Graft Surgery (CABG)
- Cardiothoracic Surgery
- Fractional Flow Reserve
- Acute Coronary Syndrome (ACS)
- Acute Coronary Care
- Acute Myocardial Infarction (AMI)
- Cardiac Rehabilitation
- Angiography
- Coronary Endothelial Function
- Carotid Artery Stenosis
- Coronary Bypass Surgery
- Coronary CT Angiography
- Coronary Artery Stenting
- Cardiac Catheterization
- Central Venous Catheter Safety and Education
- Carotid Endarterectomy
- Carotid Artery Disease
Find a Treatment Center
- Cardiac Rehabilitation and Exercise
- Heart and Vascular Institute
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital